Varicose veins of the lower extremities is a problem that affects more than 60% of the world's population. The term "varicose veins" from the Latin "varix" is interpreted as "expansion". Hence the definition of the pathological condition - the expansion of the lumen of the veins of the lower extremities and pelvic organs, which significantly impedes blood flow in the vessels and, consequently, worsens the general condition of the patient. In the material below, we will consider the causes of varicose veins, possible complications of the disease and the main ways to solve the pathology.
Causes and risk factors: all are subject to this
Important:if varicose veins overtake young people under the age of 25, here the gender distribution occurs 50: 50. That is, both boys and girls are equally ill. At a more mature age, women are more likely to have varicose veins due to pregnancy and significant changes in hormonal levels that are associated with age.
If we take into account the varicose veins from the inside, then anatomically there is a dilation of the lumen of the veins due to the failure of the venous valves that regulate blood flow. Defective valves do not close completely with each heartbeat. As a result, the blood coming from the heart moves in jerks towards the lower extremities due to the force of gravity.
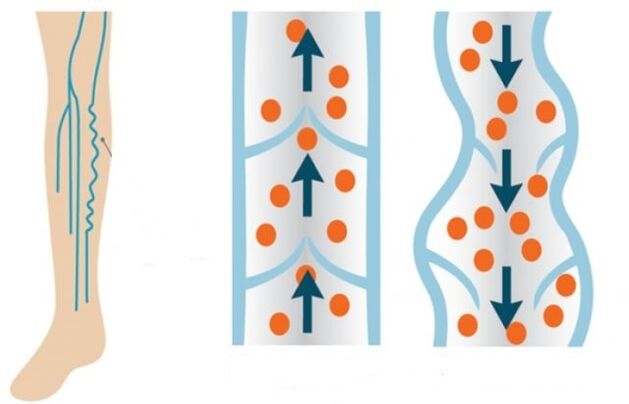
Normally, the valves should close and allow parts of the blood to flow to the legs. But, unfortunately, the blood flow enters the legs more intensively, and in the opposite direction it moves less intensively due to the same poor functioning of the valve system. Veins full of blood lose their elasticity and stretch over time.
The main predisposing factors for the development of a pathological condition of blood vessels are:
- genetic component (the disease can be transmitted by female or male lineage in the family);
- overweight;
- delayed pregnancy;
- passive lifestyle;
- excessive physical activity;
- smoking and drinking alcohol;
- hormonal disorders.
Men's problems
If we consider the causes of varicose veins, depending on the sex of the patient, then men and women differ somewhat. More precisely, each of the representatives of different sexes is prone to certain habits, which sooner or later can cause pathology of the blood vessels of the lower extremities. So, for men, the risk factors are:
- strength training with lifting weights from a squat position;
- overweight and obesity;
- unbalanced diet, which causes frequent constipation;
- pathological processes of the kidney (tumors of various etiologies);
- inguinal hernia;
- sedentary work;
- smoking and drinking alcohol.
Important:men are characterized not only by the development of varicose veins of the lower extremities, but also varicose veins of the seminal vesicle. This pathology is called varicocele. Such a condition is inherited, ie it is exclusively genetic in nature and is not prevented even by intensified preventive measures. Only 2-4% of men suffer from varicocele. The cause of the pathology is the asymmetric anatomical location and structure of the male genital organs.
Due to the fact that men suffer from false shyness or do not have time to visit a specialist at the very beginning of the disease, varicose veins are harder for them than for women.
Varicose veins of women have their own laws
For women, varicose veins are "better known" than for men. More than 80% of women suffer from vascular pathology of the legs. Moreover, the risk group includes the fairer sex who prefer this lifestyle or experience the following conditions:
- wearing tight high-heeled shoes;
- sitting or standing work;
- hereditary predisposition;
- changes in hormone levels during pregnancy or with autoimmune diseases;
- wearing too tight underwear, jeans;
- smoking;
- low percentage of fruits and vegetables in the diet (constant diet and starvation);
- love of sunbathing (frequent visits to the solarium or staying in direct sunlight);
- rapid weight gain;
- poor mobility.
Pregnancy is where the "dog is buried"
Even if the manifestations of varicose veins, the causes and treatment of which should be determined and prescribed only by a phlebologist, are not initially noticed in a woman, in 30% of cases it becomes apparent during pregnancy. Here the main trap lies in the growing fetus, and with it in the uterus, which intensively squeezes out the pelvic organs. As a result, blood circulation in the lower part of the body is significantly impaired. The return flow of blood from the legs upwards is difficult. This effect on the deep veins of the legs leads to the fact that the vessels are actively stretched both in width and length.
In addition to the growth of the uterine organ and the pressure on the vessels of the pelvic organs, varicose veins in pregnant women also develop under the influence of such factors:
- Increased blood clotting. Thus, nature insures a woman from great blood loss during childbirth. Thick blood moves more strongly through the veins.
- Increased levels of the hormone progesterone, which leads to relaxation of the muscles and blood vessels of the uterus, so that it can increase freely and without tone as the fetus grows. But at the same time, the walls of the remaining vessels relax. The veins become less elastic, and the thick blood stretches their walls even more, already weakened by progesterone.
- Increase blood pressure for better fetal oxygen supply. As a result, the body tries to quickly push thick blood through the relaxed vessels. Due to that, its volume in the legs increases.
- Low mobility of a pregnant woman with abdominal growth. This leads to blood stagnation in the legs and pelvic organs.
Complications of varicose veins
If varicose veins are not treated and not paid attention to, over time the patient can develop very serious complications that may require even full-fledged surgical intervention. In the worst case, the patient may undergo amputation of the diseased limb. Below we will consider the most common and most dangerous complications of varicose veins.
Chronic venous insufficiency
With the development of such a complication comes the active failure of the venous valves. Moreover, the pathological process is divided into four stages:
- Zero. After a hard day, the patient feels slight swelling and rare pain in the legs.
- First. A venous network of varicose veins is visualized on the surface of the skin.
- Seconds. Swollen veins with blood clots and nodules in them are clearly visible. In places of inflamed veins there is redness of the skin, itching, ulcers.
- Third. Trophic ulcers with inflamed veins form on the legs.
Important:signs of chronic venous insufficiency are itchy legs, pain, burning sensation in a prolonged sitting position, swelling, night cramps.
Superficial vein thrombophlebitis
In this case, the patient develops a tendency to form blood clots. Clots actively block the lumen of the veins, impeding blood flow. In most cases, blood clots and clots are localized in the vessels of the lower third of the thigh or the upper third of the leg. Symptoms of venous thrombophlebitis are:
- redness of the skin of the feet at the sites of clot formation;
- leg pain;
- palpation - hardening in the veins.
Important:in thrombophlebitis it is necessary to wear compression stockings. The compression formula should be chosen by a specialist - an angiosurgeon or phlebologist.
Trophic ulcer
This complication is manifested already in the later stages of venous insufficiency. First, the patient develops increased vascular permeability. A whitish seal with a varnish-like surface forms on the surface of the skin. An ulcer forms beneath it. At the slightest injury to the inflamed area, the ulcer opens and the separation of the exudate begins. The emerging wound can be secondarily infected, which leads to purulent inflammatory processes.
Important:in this condition, complete wound healing is required first, and only after that a full-fledged surgical intervention is performed to remove the affected vessels.
Pulmonary emboli
An equally dangerous complication, in which the thrombus separates from the inflamed vein and moves towards the pulmonary artery. This artery is directly involved in the organization of blood flow in a narrow circle, affecting the right ventricle of the heart. If the diameter of the detached thrombus is smaller than the lumen of the artery, then the clot moves to the branches of the pulmonary artery, causing pulmonary edema or infarction. In this case, the patient will feel significant chest pain. There will also be a wet cough mixed with blood, a rise in body temperature and weakness. If the diameter of the clot is equal to the diameter of the lumen of the pulmonary artery, then there is immediate blockage and death for the patient.
Separation of a blood clot can be initiated under the following conditions:
- performing surgical interventions;
- oncology;
- Heart Failure;
- long bed rest.
Conservative and surgical treatment
Varicose veins can be treated conservatively and surgically, depending on the stage of the pathology and the condition of the patient. In addition to conservative treatment, the use of phlebotonic drugs is indicated. Wild chestnut gels and venotonic ointments are used externally. It should be understood that conservative treatment works only in the initial stages of varicose veins.
Physical activity (walking) and wearing compression stockings have been shown as additional measures in the conservative treatment of varicose veins.
Minimally invasive and surgical methods of treatment
If the process of varicose veins and venous insufficiency has gone far, then minimally invasive or full-fledged surgical intervention is resorted to in order to improve the patient's condition. Minimally invasive methods of intervention include the following:
- Sclerotherapy. In this case, a special sclerosing drug is injected into the lumen of the patient's varicose vein using a thin insulin needle. The injected substance first causes inflammation, and then sclerosis of the diseased vein. The lumen of the diseased vessel simply overgrows. The technique has a rather cosmetic effect, but does not solve the problem (cause) of the pathology itself. Relapses are possible after sclerotherapy. Contraindications for such an intervention are pregnancy, breastfeeding and intolerance to the components of the drug.
- Download. With this method, the diseased vein is removed with the thinnest probe. The peculiarity of the surgical intervention is that it is possible to remove only the diseased part of the vessel, leaving healthy parts. The operation is performed through two endoscopic punctures located on both sides of the site of the inflamed vessel. That is, scars and scars after such an intervention will not be visible.
- Microphlebectomy. Removal of diseased veins is also done through several small incisions in the skin.
- Laser coagulation. Laser exposure of diseased vessel lumen. As a result, the lumen of the vein is completely overgrown.
Full surgical intervention (abdominal surgery) is called phlebectomy. With this method, the surgeon makes a complete incision in the skin of the leg to remove the entire superficial vein. Indications for such an operation are:
- large amount of varicose veins;
- large cavity (lumen) of diseased vessels (more than 10 mm);
- thrombophlebitis;
- the presence of large varicose veins;
- formation of trophic ulcers in the patient;
- lack of efficacy of minimally invasive surgery.
Traditional methods of treatment
In the initial stages of pathology, you can also resort to folk methods of treating varicose veins. In particular, in combination with drug treatment you can use the following folk remedies:
- The tomato is green. Thin slices of vegetables are placed on the area of inflamed veins and fixed with a bandage. You need to change such applications every 2-3 hours. The course of treatment lasts until a clear improvement of the condition.
- Potato. A bandage soaked in freshly squeezed potato juice is put on the legs. Cover the top with cling film. Such applications are best done at night until the patient's condition improves.
- Vinegar. Preferably homemade. Dilute the vinegar in water (1 cup of water and 2-3 tablespoons of vinegar). The bandage is moistened in the solution and applied to the area of diseased veins. The bandage is fixed at night. You can also simply lubricate your feet with this solution at night. It has been shown to take vinegar water inside as well. Add 1 tablespoon of apple cider vinegar and a teaspoon of honey to a glass of water so that the esophagus does not burn with vinegar (the walls of the esophagus are very susceptible to acids). Drink the mixture in the morning on an empty stomach. The course of vinegar treatment is 30 days.
- Horse chestnut. Flowers of the plant in the amount of 50 gr. pour 0, 5 liters of alcohol and insist two weeks in a dark place, shaking the mixture occasionally. The finished product is filtered through a sieve and drunk three times a day, per tablespoon. The mixture was washed with water. The course of treatment is 7 days. Then a break of 14 days and again a seven-day course. Treatment according to this scheme is carried out until the infusion is completed. Then the therapy regimen can be prepared again and repeated.
- Velcro. In this case, fresh leaves of the plant are used to eliminate the disease. At night, sore feet are smeared with Vishnevski's ointment and wrapped in a burdock leaf on top. All are fixed with a bandage and placed on compression stockings. The bandage is worn for three days and then removed and everything is rinsed. In this way, it is possible to treat yourself throughout the summer, while fresh burdock grows.
Important:such treatment is contraindicated in patients with high gastric acidity.

conclusions
It is worth understanding that varicose veins are in most cases an irreversible pathology. That is why it is so important to take care of your foot health. Especially if there is a genetic predisposition for varicose veins. It is enough to give up bad habits, balance your daily diet, walk more and drink enough clean water a day. At the manifestation of the slightest signs of varicose veins, it is desirable to contact a competent phlebologist immediately in order to prevent complications of the disease. Remember, your health and internal foot health are completely up to you. And modern medicine and the hands of a professional can do wonders.























